One year ago, in the midst of studying for exams and gearing up for my summer internship, I was also thinking ahead on how I wanted to spend my last year of graduate school. I served as the Communications Chair for the HPSA Executive Board and knew that sharing my passion for health policy with my peers was among my goals for finishing my graduate experience. With that excitement, I was elected as the President of HPSA. Now, just weeks away from graduation, I wanted to share some of my reflections:
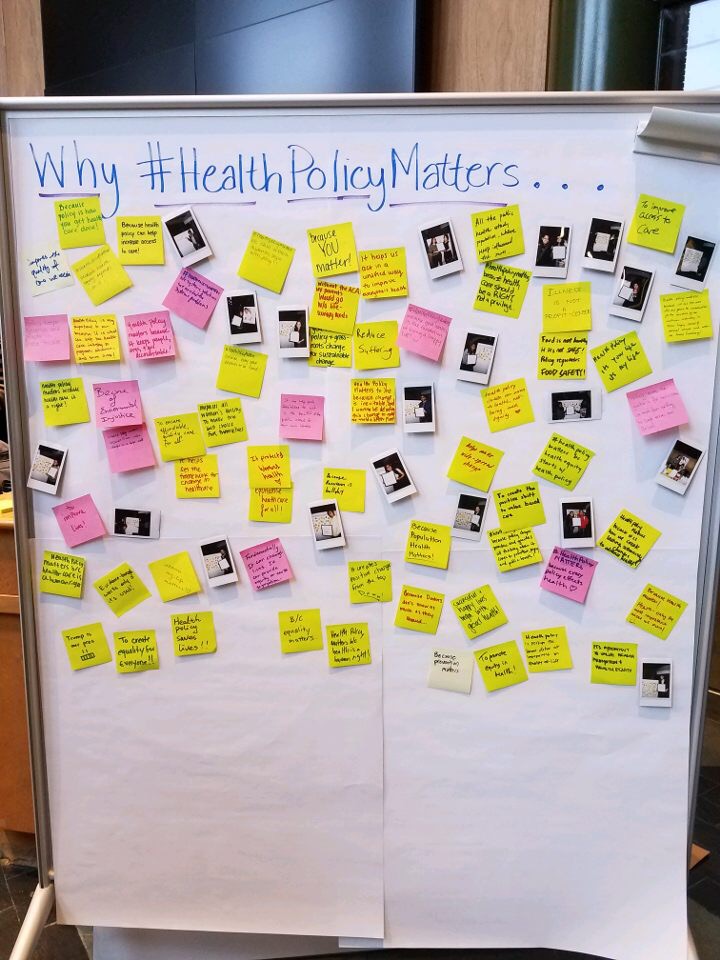
In planning for the year, many of our events revolved around the election, from baking First Lady cookies on the Presidential Election night to lining up the Second Annual #HealthPolicyMatters week with Inauguration Day. However, I was not as prepared as I thought I would be in regards to the election outcome, and HPSA was helped me to process those feelings. We quickly prepared a Post-Election Panel, inviting five faculty to share initial thoughts on what health policy would look like under the Trump Administration. The room was filled with students and community members seeking answers and the panelists did a great job of framing the issues. We were recently honored by the Public Health Student Assembly naming this as the Event of the Year! At a General Body Meeting in early 2017 we invited HPSA members for a facilitated dialogue on the implications of the new administration and concluded the meeting with the opportunity to write postcards to Senators advocating on behalf of the Affordable Care Act and other policies. And despite feeling uneasy about what was to come, we still went bowling on the eve of inauguration.
As the HPSA programming was amplified by the election results, our bond was simultaneously strengthened. We cultivated community through ice breaker activities at one of our first General Body Meetings and treated our committee members to an appreciation dinner. We also hosted a tailgate, inviting alumni and faculty attend, in collaboration with our sister student organizations, the Michigan Healthcare Executive Student Association (MHESA) and Women in Health Leadership (WiHL).
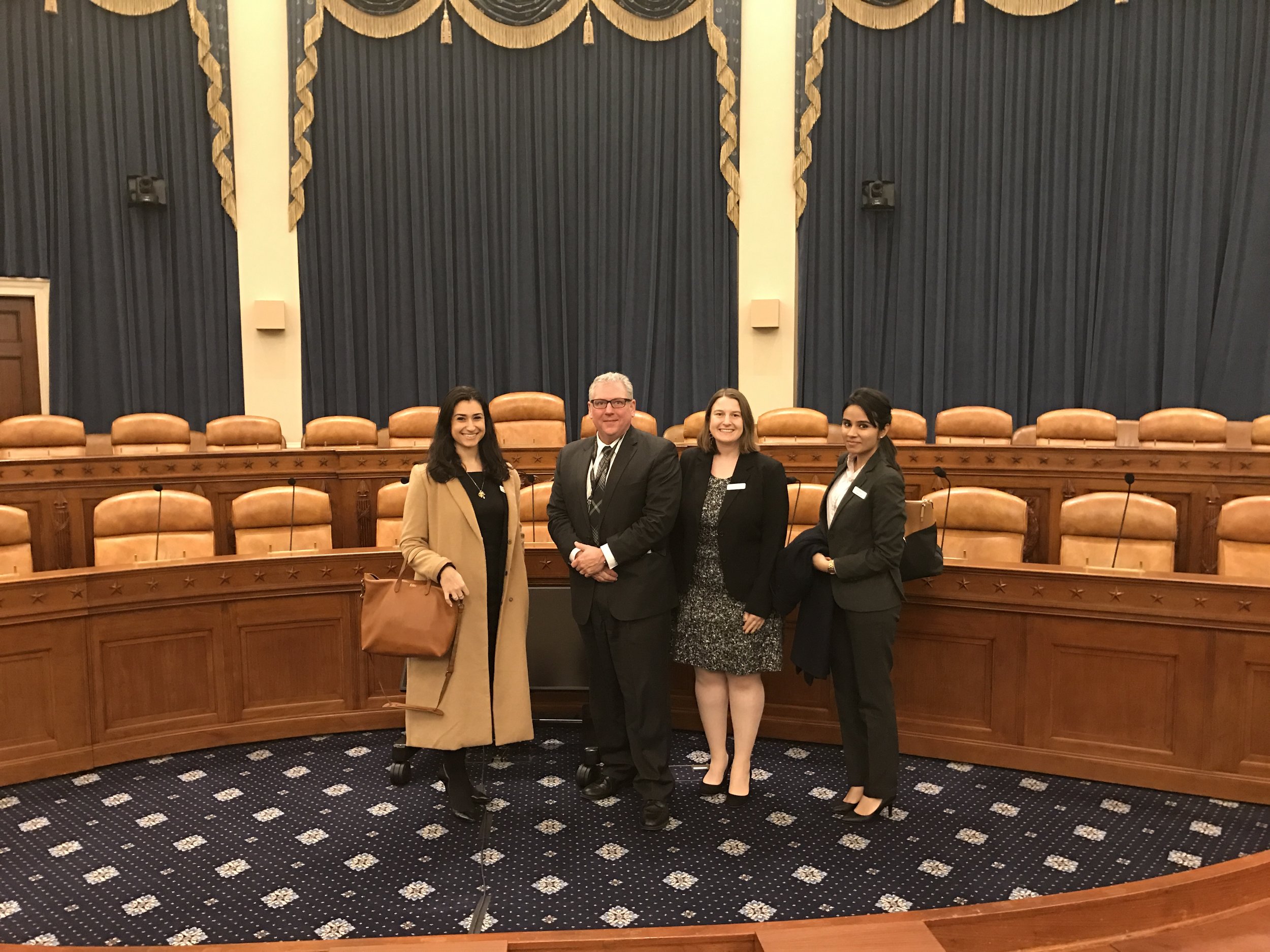
I am excited to share that we provided the opportunity for students to meet with more than nine industry leaders to join us for events throughout the year. These included speakers from academia, population health, and various levels of government for both our General Body Meetings and a Population Health coffee chat series. Additionally, we funded three students to attend the AcademyHealth National Health Policy Conference in January. These students represented the University of Michigan while networking with an array of alumni.
Please know that all of these accomplishments are not mine alone. You may have noticed that throughout this reflection, I have using the pronoun “we.” The “we” is referring to my Executive Board: Hayatt Ali, Liz Kelman, Janelle Papin, Kim Pham, and Pat Oungpasuk. I would like to share a tradition of ours and how we begin every Board meeting. Before jumping into business, everyone around the table shares something positive. We call it our rosebud. It actually began as rosebud/thorn, but we dropped the end to focus simply on the good. This tradition has been important to me as even at the most stressful points of the year, when I was dealing with a loss in my personal life or when I just had a long day, sitting down with my HPSA Board meant shifting toward positivity. Thank you to my team and phenomenal friends for your dedication to HPSA and for making this a great year. In closing out this note and this year, I will share a final rosebud with you all, a quote from one of my favorite authors, Kurt Vonnegut:
"Many people need desperately to receive this message: 'I feel and think much as you do, care about many of the things you care about, although most people do not care about them. You are not alone.'"
To my HPSA Executive Boards (past, present and future), the HPSA community, and all of the health policy nerds out there: continue caring, be persistent and remember that we are in this together. It has been an honor to serve represent HPSA and I look forward to continuing sharing why #HealthPolicyMatters in a new capacity.
Go Blue!
Haley Haddad, HPSA President