Member Dispatches from AcademyHealth 2017: Day 1
HPSA members, Marianthi Hatzigeorgiou, Liz Kelman, and Paawan Singh are at this year's AcademyHealth Conference and will be updating the blog to share their experience. Please stay tuned to hear more, and feel free to follow their live-tweets on Twitter: @Liz Kelman and @NotMaryAnthony.
L-R HPSA members: Paawan Singh, Liz Kelman, and Marianthi Hatzigeorgiou
Day 0: Each HPSA member is being hosted by a recent HMP/HPSA alum. Liz with Ruth McDonald (MPH/MPP), Marianthi with Jessica Lin (MPH ‘16) and Christopher Lee (MHSA ‘16), and Paawan with Emily Moore (MPH ‘16). Liz and Paawan met up with Emily for dinner at a Lao restaurant in Columbia Heights while Marianthi was getting to know the train and metro system between Baltimore and DC.
Day 1: The conference ran from 8am til 6pm, with a reception and student networking hour afterward. Given that we are only in town for two days, we took some liberties with our schedule to make the most of our time here! After a quick lunch break to meet with HMP alum and a photo detour to the Capitol building, we returned to the conference to hear Nancy Pelosi speak. We jumped back in to hear the second half of a panel on Reimagining Health Equity.
The closing plenary discussed innovation in healthcare. We met up with Megan Collado (MPH ‘12) at the reception, but skipped out early to head to the Supreme Court for the protest against Trump’s immigration ban. What a day!
Here are some of the take-away’s from the conference so far:
Living in a VUCA World
Lisa Simpson, President and CEO of AcademyHealth, kicked off the conference with an introduction to the current landscape of healthcare. Unfortunately, no one knows what will happen to existing laws, or predict what might happen in the very near future. The word “VUCA” (Volatile, Uncertain, Complex and Ambiguous; “cray” as the young folk say) describes the current situation, which is a little discerning when you consider how many lives are at stake. As Nancy Pelosi would later address, Repeal & Replace could cost over 32 million Americans their health insurance by 2023. Many fellow tweeters and attendees spent some time worrying about the implications of VUCA realities; and set a stage, if not of panic, of concern and prioritization for current policies.
X-Rays don’t show immigration status
Though the AcademyHealth conference focuses on healthcare policy and health services research, health policy is more than just healthcare policy. To quote Simpson, “Immigration policy is health policy that will affect us in a very real way.” (But all you SPH students know that!)
What’s Reality Without Some Fact?
Evidence-based policy is still important, even though policymakers (particularly in proposed Repeal & Replace solutions) seem to put less faith in evidence and more in...alternative facts, or predisposed notions on healthcare. (see tweet exchange) There’s a worry that stories, albeit powerful, should not be used in place of data to strengthen arguments: “the plural of anecdote is not data”, rather, we should consider marrying the two to create the most effective policies
Sen. Bill Cassidy’s Proposal: #SAD!
Simpson introduced Sen. Bill Cassidy (R-LA) to speak. He had helped author the Patient Freedom Act of 2017, and we were really interested to hear about the alt-solutions to the ACA. Though Paawan and Marianthi only have had a semester of HMP/SPH education, it took no time for them to start looking quizzically around the room. Thankfully, they weren’t the only ones. In a room of educated experts in health policy and basic economic understandings of the healthcare market, Cassidy quickly lost the traction he was hoping to gain from the audience. The solution wants to remove mandates yet keep the same amount of people covered while covering their preexisting conditions. Women, expect to naturally pay more than men because, ya know, “they’re all having children”. States, valued as the core of America per the GOP (his words, not ours), should keep the ACA if they want to, or get rid of it, or use federal money, or their own! Everyone wins!! O__o Feeling like we were oddly at a taping of Oprah, we looked to Twitter to see what others thought of the “have your cake and eat it, too” solution. Thankfully, we weren’t the only ones unimpressed. Hoping that, should Repeal & Replace be our next reality, we have something a little more realistic to consider.
Bills, Bills, Bills….& Drugs, Drugs, Drugs
The drug pricing panel offered us insight into how we could possible reformat payment policies to lower the costs of drugs. What’s the new trend? Value-Based Care. (Value-Based Care is basically the new brunch of the pharma pricing). Drug pricing wants to incorporate more value-based care, but also, per the Bristol Meyer Squibb panelist, any changes should go to experts who “really think about that” before implementation. Though the facts and figures are available in predicting how value-based care can benefit consumers and overall health spending, there is often a hesitation from manufacturers to readily accept these payments. However, staying with the status quo is not a safe fallback.
On rising prices, the consumer perspective was, “Innovation is useless if no one can afford it”. What do you consider in such considerations, then? Spending is the wrong metric- it's easy to reduce spending alone. The goal is efficient healthcare delivery and maximum value. There was considerable time spent discussing quality metrics that should be considered and reconsidered before price adjustments were implemented. However, there again was some discrepancy among the panel of what constitutes as quality metrics and how much time can be allotted here before consumers were negatively affected.
Mama MACRA, Here we go again
Liz was able to attend the “MACRA: What Now?” panel discussion. There was a lot of insight and focus again on value-based care: specifically, how quality metrics are needed to successfully implement or evaluate new payment models. Kate Baicker, a panel speaker, noted how “Healthcare policy tries to balance promoting competition and care coordination”. How can they or do they work in aggregate? There is still a lot to consider and many evaluation challenges ahead for MACRA, but some great takeaway points.
A lot of the discussion was centered around the idea of incentivizing high value care for patients and aligning that with payment systems, echoing many of the points considered at the University of Michigan’s Center for Value-Based Insurance Design.
#HMPeverywhere #MichiganMafia
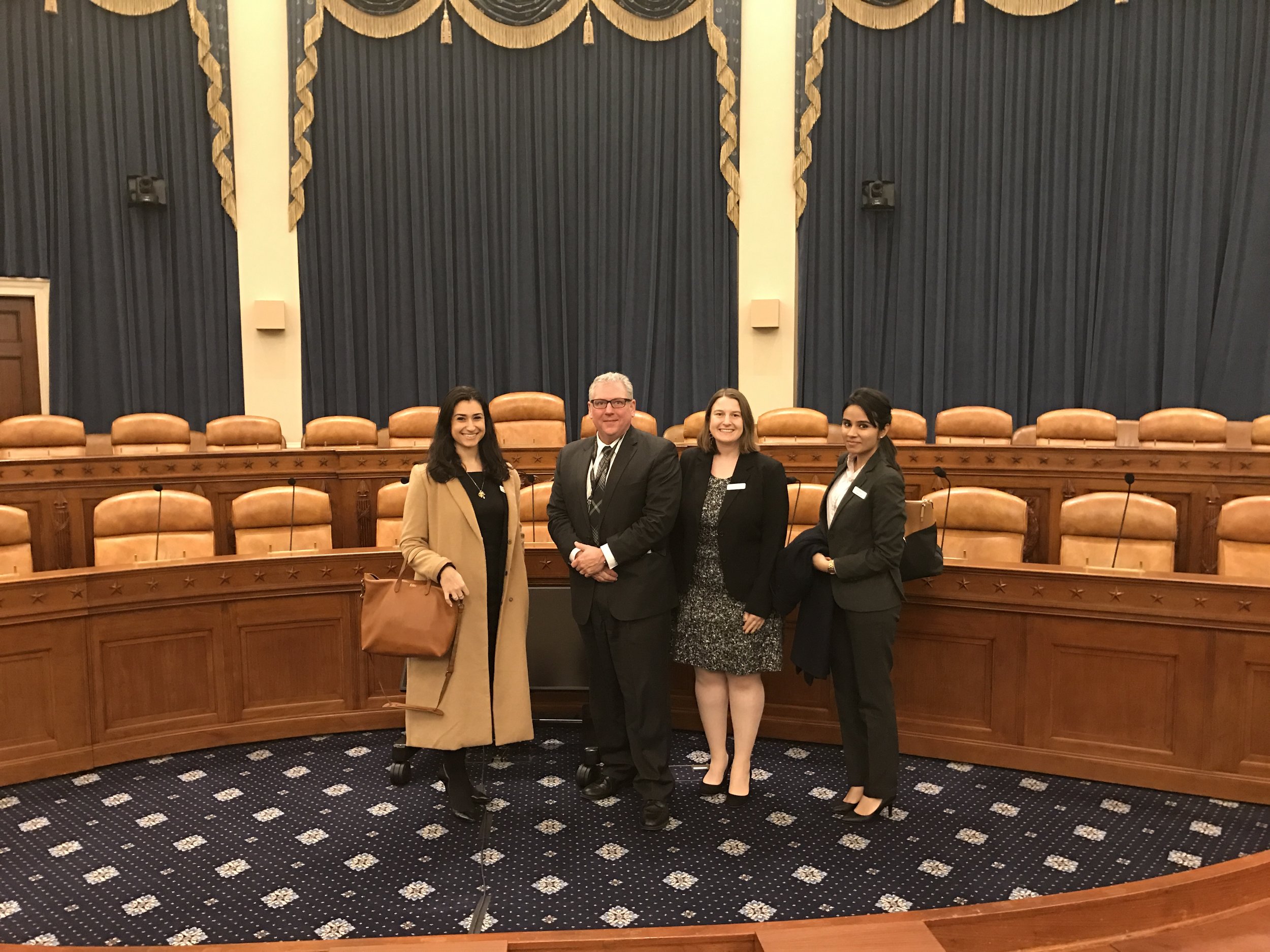
As mentioned earlier, we were fortunate enough to use the lunch break for a quick dash to the Hill to meet a fellow HMP alum. Daniel Ochylski, an SPH alum and current Robert Wood Johnson Health Policy Scholar in the Ways and Means Committee, was kind enough to take the time out of his day to chat for awhile in the staff meeting room. We discussed the intimate association between advocacy groups and committees, the uncertainty of the current administration, how the most important thing anyone can be doing is getting involved. Later, he told us about his PhD research that involved developing a simulation program for the practical training of nurses; training of home-care workers in an attempt to establish qualification standards. Before we had to head back, he gave us a tour to the #room(s)whereithappens!
L-R: Marianthi Hatzigeorgiou, Dan Ochylski, Liz Kelman, and Paawan Singh
Throughout the rest of the day, they were lucky to meet with Megan Collado (MPH ‘12) and discussed her role with AcademyHealth, Randel Richner (MPH ‘90), Donna Friedsam (MPH., ‘90) Health Policy Programs Director at the University of Wisconsin Population Health Institute, and Dr. Neil S. Fleming (VP of Quantitative Sciences, Baylor Scott & White Health).
Innovations Disrupting Healthcare
Going ahead, we hope to see a shift from in house hospital and clinic healthcare delivery models to a delivery system that uses technology to care for patients in their homes. Healthcare startups and innovators are set to gradually begin disrupting parts of the brick and mortar hospital system. The imminent change in healthcare landscape sees consumers playing the central role in steering ahead (more care outside hospitals, home-care, technology aided early interventions, etc.) The evolution is not going to wait for providers or policies to drive. Consumers are now equipped with more information than ever before, and have changing healthcare needs that are being met by innovators. “Healthcare is a team sport” (Nancy Gagliano) and partnership is key to enabling effective change.
Chronic care patients can hope to benefit from this and as, Dr. M. Christopher Gibbons said, “the term ‘noncompliant patient’ needs to be eradicated and we need to transition to thinking of patients as compliant but lacking the right tools to succeed. Rasu Shrestha, a panel member, wants chronic-care patients discharged with the technology to help prevent their readmission. The best part is that it’s already happening!